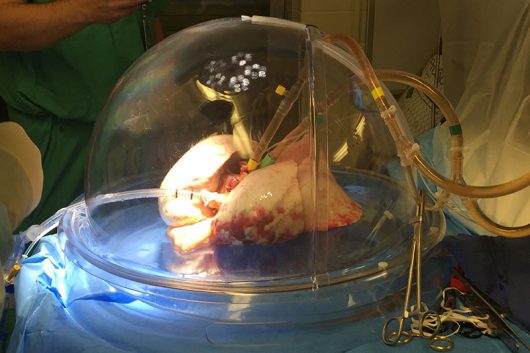
A lung undergoes ex-vivo lung perfusion at the Wexner Medical Center. Credit: Courtesy of Ohio State
It looks like a scene from a sci-fi movie — a plastic dome breathes life into a pair of lungs, which will then breathe life into a dying patient.
This emerging process, called ex-vivo lung perfusion, is part of a trial that could significantly increase the number of working lungs for transplantation. The Wexner Medical Center at Ohio State is one of 17 institutions in the U.S. to test the EVLP treatment.
“Expanding the number of lifesaving and life-enhancing lung transplants is limited by the number of available donors and the quality of the donated organs,” Dr. Bryan Whitson, director of the lung transplant program, said in a news release. “Having the ability to more adequately evaluate potential donor organs and to even repair or resuscitate them is a game changer for lung transplantation.”
Because of the fragility of lungs, 80 percent of donor lungs are unusable.
“Normally, things kind of unfold pretty quickly with donors,” said Amy Pope-Harman, a pulmonologist who is part of the Wexner Center’s transplant team. “We don’t really have the option to see how things will unfold over time, so often we have to walk away.”
EVLP treatment could potentially expand the donor-lung pool.
“Those (previously unusable) lungs could potentially be tuned up, and we’ve never had a mechanism to be able to do that,” Pope-Harman said. “And now we have this ex-vivo perfusion that we can try, and it gives us some time.”
After being placed into an incubator, the lungs steadily inflate from a circuit that removes excess water and inserts nutrients. As the lungs sit for three to six hours, its oxygen levels and airway pressure are constantly assessed.
While in the machine, “we can assess how well the lungs are working … and have a better idea of how well they’re going to work with the patient,” Pope-Harman said.
Due to the nature of lung transplants, some patients wait years for a match. According to the Wexner Center, OSU’s average wait time for a lung transplant is 1.9 months, compared to the national median of 4.2 months. Although some patients come in and immediately receive their transplants, others are forced to wait for their new lungs.
“That’s the part that brings you home and humanizes you as you’re realizing this person is very slowly dying in front of your eyes,” Pope-Harman said. “So it feels great knowing that there could be a lung come sooner for them than otherwise.”
Though EVLP treatment is still under evaluation, it could one day impact all patients across the country in need of a lung transplant.
“I can’t tell you how gratifying it is,” Pope-Harman said. “I always knew that the potential was there, and I knew that we could help people, but we just couldn’t quite get it off the ground, and to have that now happen with a new team is just elating. It’s really exciting.”
Correction, Sept. 21: A previous version of this article listed the average wait time as 1 year and 9 months. In fact, it is 1.9 months. Additionally, the national median wait time has been corrected.


